At the end of the decade it is the time to reflect on what has happened in the past before planning for the future. As always, the hottest topic in health care is the status of the emergency care services, and we have the data – it is public.
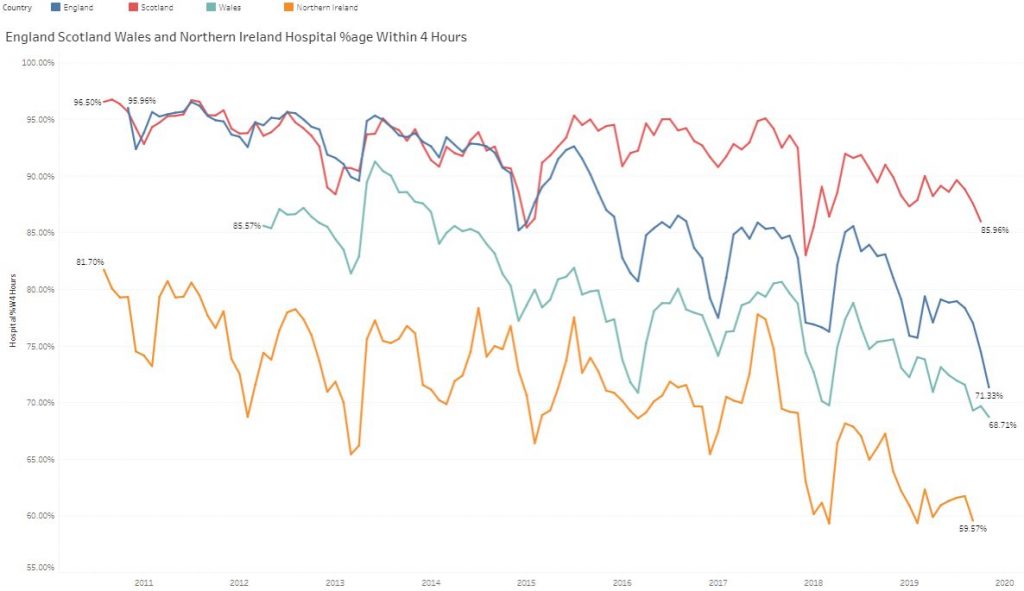 This shows the last 9 years of aggregate, monthly data for Scotland (red), England (blue), Wales (teal) and N.Ireland (orange). It does not take a data scientist and a supercomputer to interpret – there is a progressive system-wide progressive deterioration year-on-year. The winter dips are obvious and the worst of these affect all four countries indicating a systemic cause … the severity of the winter weather/illness cycle -i.e. the Flu Season.
This shows the last 9 years of aggregate, monthly data for Scotland (red), England (blue), Wales (teal) and N.Ireland (orange). It does not take a data scientist and a supercomputer to interpret – there is a progressive system-wide progressive deterioration year-on-year. The winter dips are obvious and the worst of these affect all four countries indicating a systemic cause … the severity of the winter weather/illness cycle -i.e. the Flu Season.
What this chart also says is that all the effort and money being expended in winter planning is not working well enough – and the nagging question is “Why not?”
Many claim that it is the predicted demographic “time bomb” … but if it is predicted then how come it has not been mitigated?
Many claim that it is a growing funding gap … but most NHS funding is spent on staff and and training nurses, doctors and allied health professionals (AHPs) takes time. Again, a predicted eventuality that has not been mitigated.
This looming crisis in a lack of heath care workers is a global health challenge … and is described by Mark Britnell in “Human – Solving the global workforce crisis in healthcare“.
Mark was the CEO of University Hospitals Birmingham from 2000 and has worked for KPMG since 2009 in a global health role so is well placed to present a strategic overview.
But, health care workers deliver care to patients – one at a time. They are not responsible for designing the system of health care delivery; or ensuring all the pieces of that vast jigsaw link up and work in a synchronised way; or for the long term planning needed to mitigate the predictable effects of demographic drift and technology advances.
Who is responsible for that challenge and are they adequately trained to do it?
The evidence would appear to suggest that there is a gap that either no one has noticed or that no one is prepared to discuss. An Undiscussable?
The global gap in the healthcare workforce is predicted to be about 20% by 2030. That is a big gap to fill because with the NHS workforce of 1.3 million people – that implies training 260,000 new staff of all types in the next 10 years, in addition to replacing those that leave.
Assuming the processes and productivity stay as they are now.
So, perhaps there is a parallel approach, one that works more quickly and a lower cost.
When current health care processes are examined through a flow engineering lens they are found to be poorly designed. They are both ineffective (do not reliably deliver the intended outcome) and inefficient (waste a lot of resources in delivering any outcome). Further examination reveals that the processes have never been designed … they have evolved.
And just because something is described as current practice does not prove that it is good design.
An expected symptom of a poorly designed process is a combination of chronic queues, delays, chaos, reactive fire-fighting and burnout. And the assumed cause is often lack of resources because when extra resource is added the queues and chaos subsides, for a while.
But, if the unintentional poor design of the process is addressed then a sequence of surprising things can happen. The chaos evaporates immediately without any extra resources. A feeling of calm is restored and the disruptive fire-fighting stops. The health care workers are able to focus on what they do best and pride-in-work is restored. Patient experience improves and staff feel that feedback and become more motivated. The complaining abates, sickness and absence falls, funded-but-hard-to-recruit-to posts are refilled and there are more hands on the handle of a more efficient/effective/productive pump. The chronic queues and delays start to melt away – as if by magic.
And if that all sounds totally impossible then here are a couple of recent, real-world case studies written by different teams in different cities in different parts of the UK. One from cancer care and one from complex diabetic care.
They confirm that this chaos-to-calm transformation is possible.
So, is there a common thread that links these two examples?
Yes, there is, and once again the spotlight is shone on the Undiscussable Gap … the fact that the NHS does not appear to have the embedded capability to redesign itself.
There is a hidden workforce gap that none of the existing programmes will address – because it is not a lack of health care workers – it is a lack of appropriately trained health care manager-designers.
The Undiscussable Elephant Is In The Room … the Undiscussable Emperor Has No Clothes.
And if history teaches us anything, Necessity is the Mother of Innovation and the chart at the top of the page shows starkly that there is an Growing Urgent Necessity.
And if two embedded teams can learn this magic trick of flipping chaos into calm at no cost, then perhaps others can too?
Welcome to the New Decade of Hope and Health Care Systems Engineering.
