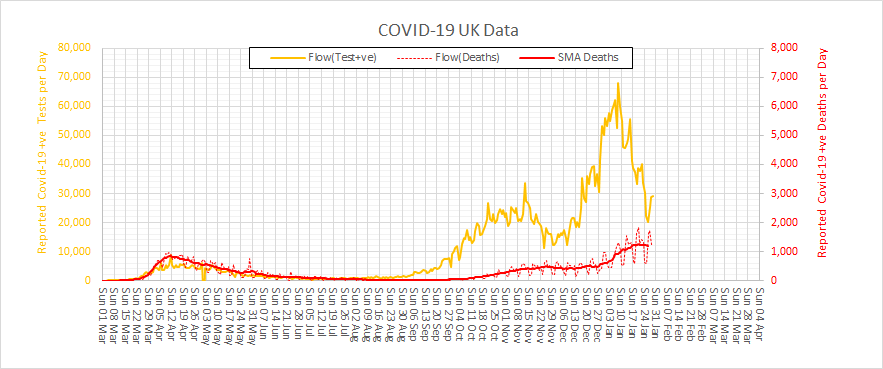
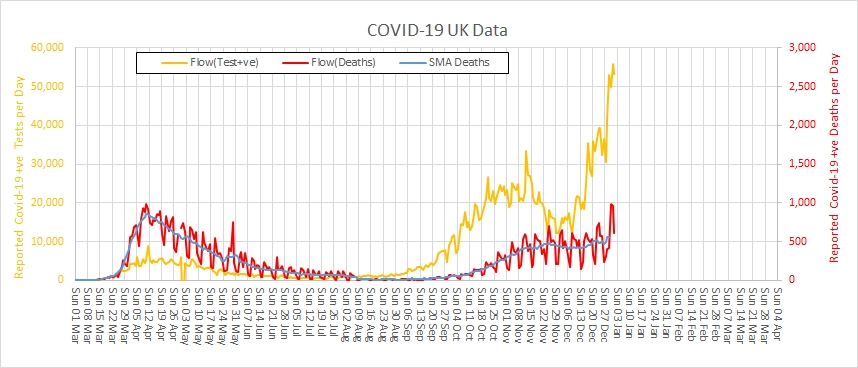
It is New Year 2021 and the spectre of COVID-4-Christmas came true. We are now in the depths of winter and in the jaws of the Third Wave. What happened? Let us look back at the UK data for positive tests and deaths to see how this tragic story unfolded.
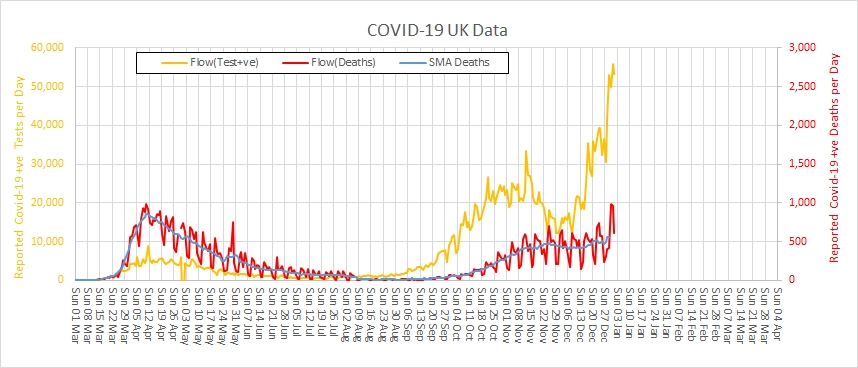
There was a Second Wave that started to build when Lock-down I was relaxed in July 2020. And it looks like Lock-down II in November 2020 did indeed have a beneficial effect – but not as much as was needed. So, when it too was relaxed at the start of December 2020 then … infections took off again … even faster than before!
That is the nature of epidemics and of exponential growth. It seems we have not learned those painful lessons well enough.
And we all so desperately wanted a more normal Xmas that we conspired to let the COVID cat out of the bag again. The steep rise in positive tests is real and we know that because a rise in deaths is following about three weeks behind. And that means hospitals have filled up again.
Are we back to square one?
The emerging news of an even more contagious variant has only compounded our misery, but it is hard to separate the effect of that from all the other factors that are fuelling the Third Wave.
Is there no end to this recurring nightmare?
The short answer is – “It will end“. It cannot continue forever. All epidemics eventually burn themselves out when there are too few susceptible people left to infect and we enter the “endemic” phase. When that happens the R number will gravitate to 1.0 again which some might find confusing. The confusion is caused by mixing up Ro and Rt.
How close are we to that end game?
Well, we are certainly a lot closer than we were in July 2020 because millions more people have been exposed, infected and recovered and many of those were completely asymptomatic. It is estimated that about a third of those who catch it do not have any symptoms – so they will not step forward to be tested and will not appear in the statistics. But they can unwittingly and silently spread the virus while they are infectious. And many who are symptomatic do not come get tested so they won’t appear in the statistics either.
And there are now two new players in the COVID-19 Game … the Pfizer vaccine and the Oxford vaccine. They are the White Knights and they are on our side.
Hurrah!
Now we must manufacture, distribute and administer these sickness-and-death-preventing vaccines to 65 million people as soon as possible. That alone is a massive logistical challenge when we are already fighting battles on many fronts. It seems impossible.
Or do we?
It feels obvious but is it the most effective strategy? Should we divert our limited, hard-pressed, exhausted health care staff to jabbing the worried-well? Should we eke out our limited supplies of precious vaccine to give more people a first dose by delaying the second dose for others?
Will the White Knights save us?
The short answer is – “Not on their own“.
The maths is simple enough.
Over the last three weeks we have, through Herculean effort, managed to administer 1 million first doses of the Pfizer vaccine. That sounds like a big number but when put into the context of a UK population of 65 million it represents less than 2% and offers only delayed and partial protection. The trial evidence confirmed that two doses of the Pfizer vaccine given at a three week interval would confer about 90% protection. That is the basis of the licence and the patient consent.
So, even if we delay second doses and double the rate of first dose delivery we can only hope to partially protect about 2-3% of the population by the end of January 2021. That is orders of magnitude too slow.
And the vaccines are not a treatment. The vaccine cannot mitigate the fact that a large number of people are already infected and will have to run the course of their illness. Most will recover, but many will not.
So, how do we get our heads around all these interacting influences? How do we predict how the Coronavirus Game is likely to play out over the next few weeks? How do we decide what to do for the best?
I believe it is already clear that trying to answer these questions using the 1.3 kg of wetware between our ears is fraught with problems.
We need to seek the assistance of some hardware, software and some knowledge of how to configure them to illuminate the terrain ahead.
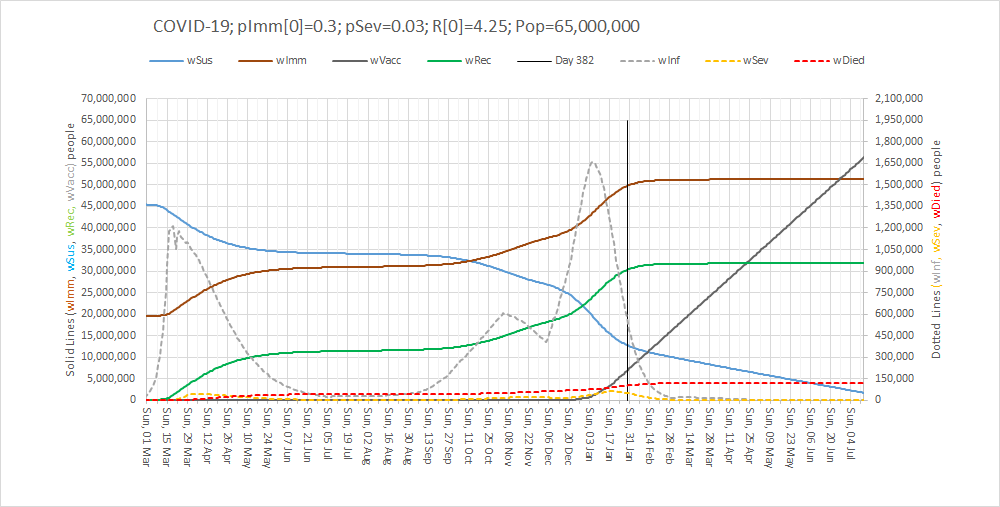
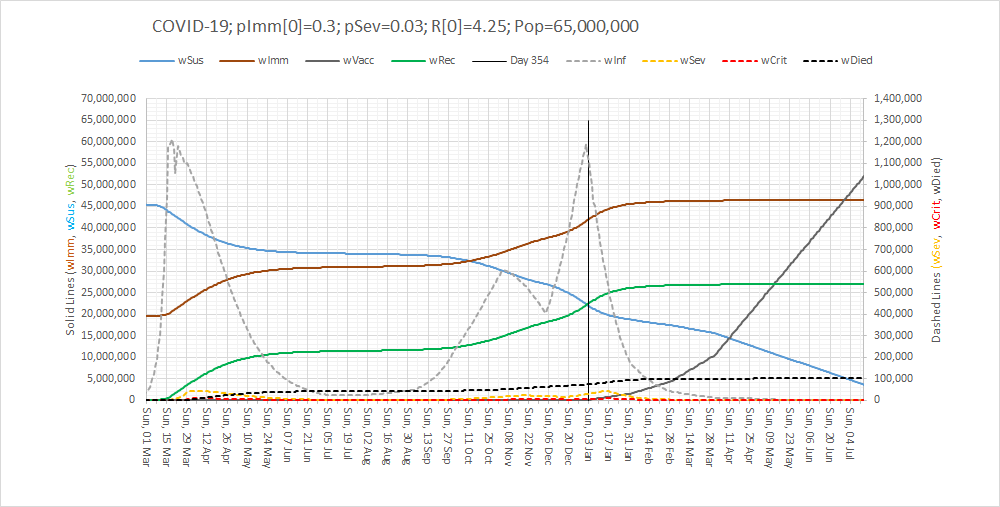
Here is what the updated SEIR-V model suggests will happen if we continue with the current restrictions and the current vaccination rate. I’ve updated it with the latest data and added a Vaccination component.
The lines to focus on are the dotted ones: grey = number of infected cases, yellow = number ill enough to justify hospital treatment, red = critically ill and black = not survived.
The vertical black line is Now and the lines to the right of that is the most plausible prediction.
It says that a Third Wave is upon us and that it could be worse than the First Wave. That is the bad news. The good news is that the reason that the infection rate drops is because the epidemic will finally burn itself out – irrespective of the vaccinations.
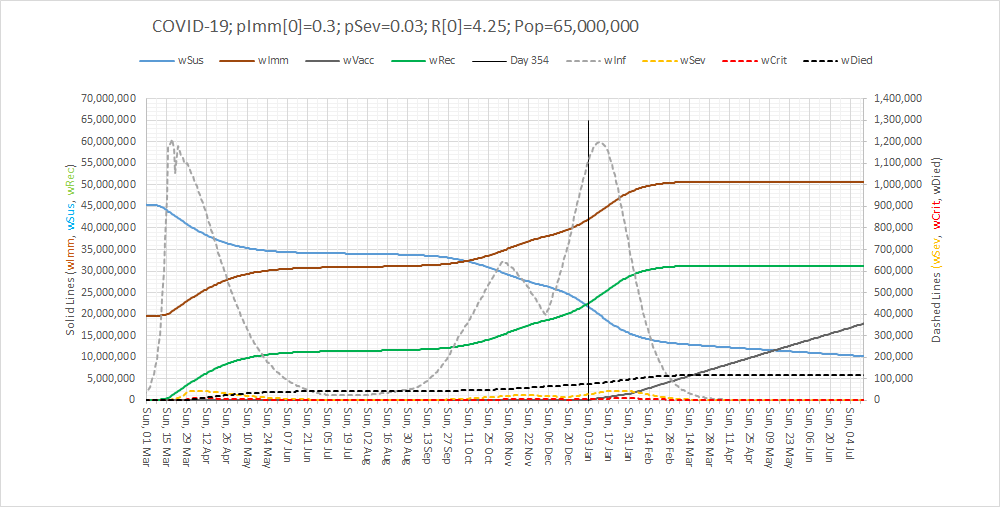
So, it would appear that the White Knights cannot rescue us on their own … but we can all help to accelerate the final phase and limit the damage – if we all step up and pull together, at the same time and in the same direction.
We need a three-pronged retaliation:
- Lock-down: “Stay at home. Protect the NHS. Save Lives”. It worked in the First Wave and it will work in the Third Wave.
- Care in the Community: For those who will become unwell and who will need the support of family, friends, neighbours and the NHS.
- Volunteer to Vaccinate: To protect everyone as soon as is practically feasible.
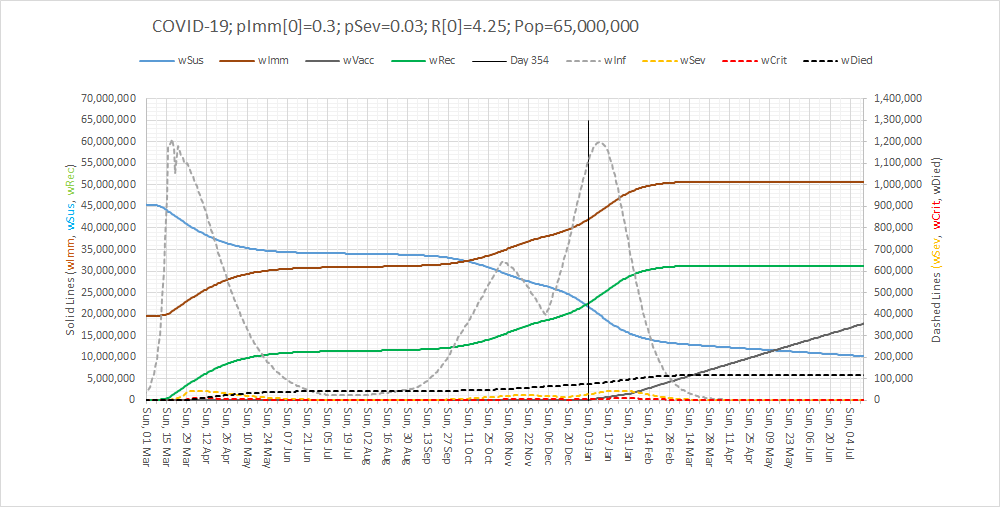
Here is what it could look like. All over by Easter.
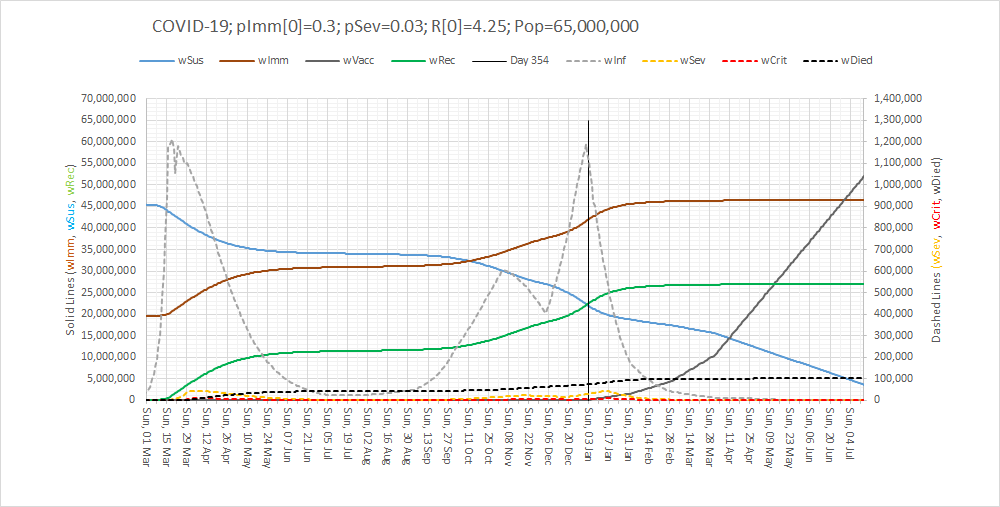
There is light at the end of the tunnel. The end is in sight. We just have to pull together in the final phase of the Game.
PS. For those interested in how an Excel-based SEIR-V model is designed, built and used here’s a short (7 minute) video of the highlights:
This is health care systems engineering (HCSE) in action.
And I believe that the UK will need a new generation of HCSEs to assist in the re-designing and re-building of our shattered care services. So, if you are interested then click here to explore further.