This week saw the publication of a landmark paper – one that will bring hope to many. A paper that describes the first step of a path forward out of the mess that healthcare seems to be in. A rational, sensible, practical, learnable and enjoyable path.
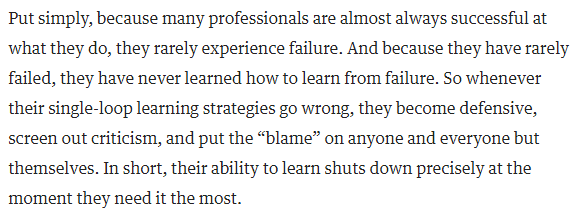
This week I also came across an idea that triggered an “ah ha” for me. The idea is that the most rapid learning happens when we are making mistakes about half of the time.
And when I say ‘making a mistake’ I mean not achieving what we predicted we would achieve because that implies that our understanding of the world is incomplete. In other words, when the world does not behave as we expect, we have an opportunity to learn and to improve our ability to make more reliable predictions.
And that ability is called wisdom.
When we get what we expect about half the time, and do not get what we expect about the other half of the time, then we have the maximum amount of information that we can use to compare and find the differences.
Was it what we did? Was it what we did not do? What are the acts and errors of commission and omission? What can we learn from those? What might we do differently next time? What would we expect to happen if we do?
And to explore this terrain we need to see the world as it is … warts and all … and that is the subject of the landmark paper that was published this week.
The context of the paper is improvement of cancer service delivery, and specifically of reducing waiting time from referral to first appointment. This waiting is a time of extreme anxiety for patients who have suspected cancer.
It is important to remember that most people with suspected cancer do not have it, so most of the work of an urgent suspected cancer (USC) clinic is to reassure and to relieve the fear that the spectre of cancer creates.
So, the sooner that reassurance can happen the better, and for the unlucky minority who are diagnosed with cancer, the sooner they can move on to treatment the better.
The more important paragraph in the abstract is the second one … which states that seeing the system behaviour as it is, warts-and-all, in near-real-time, allows us to learn to make better decisions of what to do to achieve our intended outcomes. Wiser decisions.
And the reason this is the more important paragraph is because if we can do that for an urgent suspected cancer pathway then we can do that for any pathway.
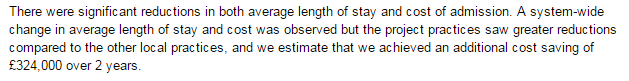
The paper re-tells the first chapter of an emerging story of hope. A story of how an innovative and forward-thinking organisation is investing in building embedded capability in health care systems engineering (HCSE), and is now delivering a growing dividend. Much bigger than the investment on every dimension … better safety, faster delivery, higher quality and more affordability. Win-win-win-win.
The only losers are the “warts” – the naysayers and the cynics who claim it is impossible, or too “wicked”, or too difficult, or too expensive.
Innovative reality trumps cynical rhetoric … and the full abstract and paper can be accessed here.
So, well done to Chris Jones and the whole team in ABMU.
And thank you for keeping the candle of hope alight in these dark, stormy and uncertain times for the NHS.