Innovation means anything new and new ideas spread through groups of people in a characteristic way that was described by Everett Rogers in the 1970’s.
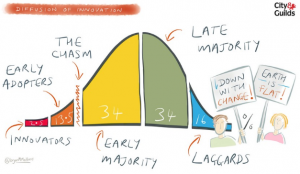 The evidence showed that innovation started with the small minority of innovators (about 2%) and diffuses through the population – first to the bigger minority called early adopters.
The evidence showed that innovation started with the small minority of innovators (about 2%) and diffuses through the population – first to the bigger minority called early adopters.
Later, it became apparent that the diffusion path was not smooth and that there was a chasm into which many promising innovations fell and from which they did not emerge.
If this change chasm can be bridged then a tipping point is achieved when wider adoption by the majority becomes much more likely.
And for innovations that fundamentally change the way we live and work, this whole process can take decades! Generations even.
Take mobile phones and the Internet as good examples. How many can remember life before those innovations? And we are living the transition to renewable energy, artificial intelligence and electric cars.
So, it is very rewarding to see growing evidence that the innovators who started the health care improvement movement back in the 1990’s, such as Dr Don Berwick in the USA and Dr Kate Silvester in the UK, have grown a generation of early adopters who now appear to have crossed the chasm.
The evidence for that can be found on the NHS Improvement website – for example the QSIR site (Quality, Service Improvement and Redesign).
Browsing through the QSIR catalogue of improvement tools I recognised them all from previous incarnations developed and tested by the NHS Modernisation Agency and NHS Institute for Innovation and Improvement. And although those organisations no longer exist, they served as incubators for the growing community of healthcare improvement practitioners (CHIPs) and their legacy lives on.
This is all good news because we now also have a new NHS Long Term Plan which sets out an ambitious vision for the next 10 years and it is going to need a lot of work from the majority of people who work in the NHS to deliver. That will need capability-at-pace-and-scale.
And this raises some questions:
Q1: Will the legacy of the MA and NHSi scale to meet the more challenging task of designing and delivering the vision of a system of Integrated Care Systems (ICS) that include primary care, secondary care, community care, mental health and social care?
Q2: Will some more innovation be required?
If history is anything to go by, then I suspect the the answers will be “Q1: No” and “Q2: Yes”.
Bring it on!