Sometimes change is dramatic. A big improvement appears very quickly. And when that happens we are caught by surprise (and delight).
Sometimes change is dramatic. A big improvement appears very quickly. And when that happens we are caught by surprise (and delight).
Our emotional reaction is much faster than our logical response. “Wow! That’s a miracle!“
Our logical Tortoise eventually catches up with our emotional Hare and says “Hare, we both know that there is no such thing as miracles and magic. There must be a rational explanation. What is it?“
And Hare replies “I have no idea, Tortoise. If I did then it would not have been such a delightful surprise. You are such a kill-joy! Can’t you just relish the relief without analyzing the life out of it?“
Tortoise feels hurt. “But I just want to understand so that I can explain to others. So that they can do it and get the same improvement. Not everyone has a ‘nothing-ventured-nothing-gained’ attitude like you! Most of us are too fearful of failing to risk trusting the wild claims of improvement evangelists. We have had our fingers burned too often.“
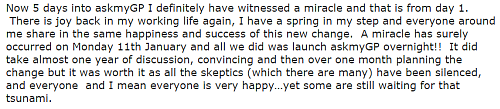
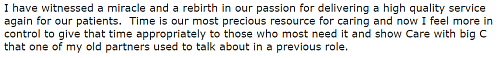
The apparent miracle is real and recent … here is a snippet of the feedback:
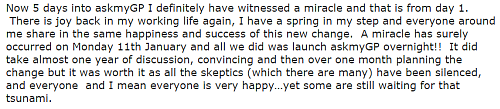
Notice carefully the last sentence. It took a year of discussion to get an “OK” and a month of planning to prepare the “GO”.
That is not a miracle and some magic … that took a lot of hard work!
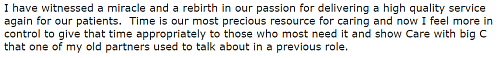
The evangelist is the customer. The supplier is an engineer.
The context is the chronic niggle of patients trying to get an appointment with their GP, and the chronic niggle of GPs feeling overwhelmed with work.
Here is the back story …
In the opening weeks of the 21st Century, the National Primary Care Development Team (NPDT) was formed. Primary care was a high priority and the government had allocated £168m of investment in the NHS Plan, £48m of which was earmarked to improve GP access.
The approach the NPDT chose was:
harvest best practice +
use a panel of experts +
disseminate best practice.
Dr (later Sir) John Oldham was the innovator and figure-head. The best practice was copied from Dr Mark Murray from Kaiser Permanente in the USA – the Advanced Access model. The dissemination method was copied from from Dr Don Berwick’s Institute of Healthcare Improvement (IHI) in Boston – the Collaborative Model.
The principle of Advanced Access is “today’s-work-today” which means that all the requests for a GP appointment are handled the same day. And the proponents of the model outlined the key elements to achieving this:
1. Measure daily demand.
2. Set capacity so that is sufficient to meet the daily demand.
3. Simple booking rule: “phone today for a decision today”.
But that is not what was rolled out. The design was modified somewhere between aspiration and implementation and in two important ways.
First, by adding a policy of “Phone at 08:00 for an appointment”, and second by adding a policy of “carving out” appointment slots into labelled pots such as ‘Dr X’ or ‘see in 2 weeks’ or ‘annual reviews’.
Subsequent studies suggest that the tweaking happened at the GP practice level and was driven by the fear that, by reducing the waiting time, they would attract more work.
In other words: an assumption that demand for health care is supply-led, and without some form of access barrier, the system would be overwhelmed and never be able to cope.
The result of this well-intended tampering with the Advanced Access design was to invalidate it. Oops!
To a systems engineer this is meddling was counter-productive.
The “today’s work today” specification is called a demand-led design and, if implemented competently, will lead to shorter waits for everyone, no need for urgent/routine prioritization and slot carve-out, and a simpler, safer, calmer, more efficient, higher quality, more productive system.
In this context it does not mean “see every patient today” it means “assess and decide a plan for every patient today”.
In reality, the actual demand for GP appointments is not known at the start; which is why the first step is to implement continuous measurement of the daily number and category of requests for appointments.
The second step is to feed back this daily demand information in a visual format called a time-series chart.
The third step is to use this visual tool for planning future flow-capacity, and for monitoring for ‘signals’, such as spikes, shifts, cycles and slopes.
That was not part of the modified design, so the reasonable fear expressed by GPs was (and still is) that by attempting to do today’s-work-today they would unleash a deluge of unmet need … and be swamped/drowned.
So a flood defense barrier was bolted on; the policy of “phone at 08:00 for an appointment today“, and then the policy of channeling the over spill into pots of “embargoed slots“.
The combined effect of this error of omission (omitting the measured demand visual feedback loop) and these errors of commission (the 08:00 policy and appointment slot carve-out policy) effectively prevented the benefits of the Advanced Access design being achieved. It was a predictable failure.
But no one seemed to realize that at the time. Perhaps because of the political haste that was driving the process, and perhaps because there were no systems engineers on the panel-of-experts to point out the risks of diluting the design.
It is also interesting to note that the strategic aim of the NPCT was to develop a self-sustaining culture of quality improvement (QI) in primary care. That didn’t seem to have happened either.
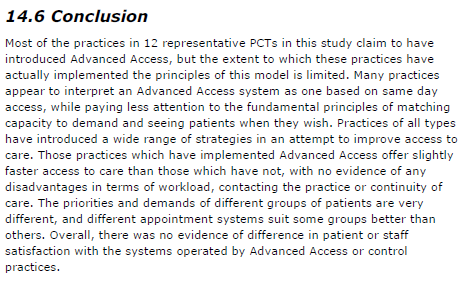
The roll out of Advanced Access was not the success it was hoped. This is the conclusion from the 300+ page research report published in 2007.
The “Miracle on Tavanagh Avenue” that was experienced this week by both patients and staff was the expected effect of this tampering finally being corrected; and the true potential of the original demand-led design being released – for all to experience.
Remember the essential ingredients?
1. Measure daily demand and feed it back as a visual time-series chart.
2. Set capacity so that is sufficient to meet the daily demand.
3. Use a simple booking rule: “phone anytime for a decision today”.
But there is also an extra design ingredient that has been added in this case, one that was not part of the original Advanced Access specification, one that frees up GP time to provide the required “resilience” to sustain a same-day service.
And that “secret” ingredient is how the new design worked so quickly and feels like a miracle – safe, calm, enjoyable and productive.
This is health care systems engineering (HCSE) in action.
So congratulations to Harry Longman, the whole team at GP Access, and to Dr Philip Lusty and the team at Riverside Practice, Tavangh Avenue, Portadown, NI.
You have demonstrated what was always possible.
The fear of failure prevented it before, just as it prevented you doing this until you were so desperate you had no other choices.
To read the fuller story click here.
PS. Keep a close eye on the demand time-series chart and if it starts to rise then investigate the root cause … immediately.
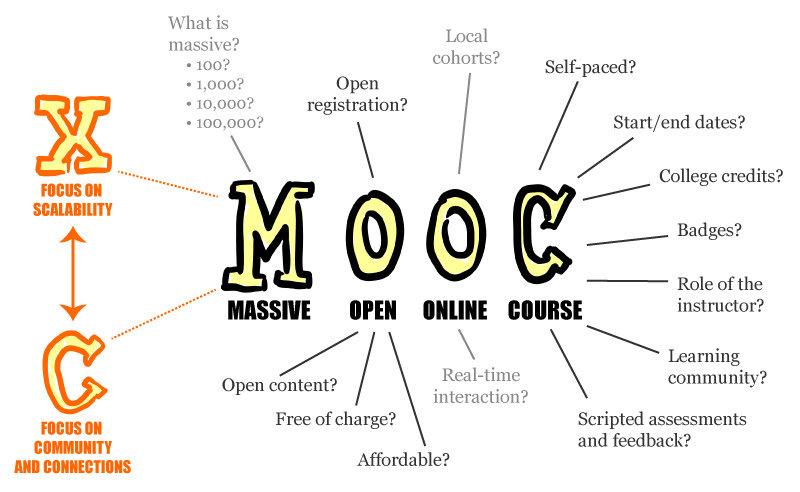
 And the good news is that there a is a MOOC for Healthcare Improvement.
And the good news is that there a is a MOOC for Healthcare Improvement.