The big wide world outside health care is stuffed with proven solutions that we can use as metaphors to guide improvement. Aviation has already given us checklists that are now an integral part of surgical services – the WHO Safer Surgery Checklist. [We will skip the uncomfortable fact that safety checklists have been used in aviation for decades longer than in surgery].
So what other aviation metaphors might be of use?
Well, one that is of particular value in these turbulent times is fly-by-wire.
When the first heavier-than-air craft, the Wright Flyer I, took off on Dec 17th, 1903 the controls were purely mechanical. The way that the pilot’s stick moved the control surfaces was only one of many innovations that the Wright brothers had created and tested over years of careful experimentation. They were self-taught, practical engineers.
Decades later the link between the pilot and the plane became replaced by a more complicated electromechanical system of sensors, processors and actuators illustrated in the diagram below. And the reason that this is necessary is that modern aircraft are bigger, faster and need to be much safer, more comfortable, more efficient, and more reliable. As fare-paying passengers we take for granted all of the advanced engineering of modern aircraft when we climb aboard. We only notice when something goes wrong which, because of the hard work of the engineers, is a very rare event.
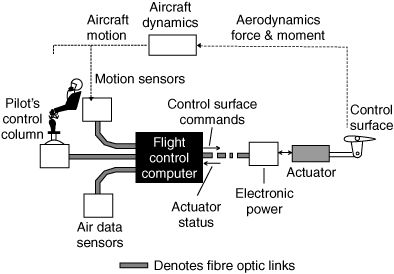
The essence of the fly-by-wire design is the triad of sensor-processor-actuator which we could translate into input-process-output (IPO) or even study-plan-do. Each of the three components is necessary and together the three components are sufficient. Interestingly, this is exactly how most biological systems are constructed – including us. Sensors, processors and effectors.
The part of the aircraft system that takes in the multi-sensory information and transforms it into signals that drive the control surfaces is NOT the pilot; it is the flight control computer (FCC). One of the sensory inputs comes from the pilot’s control stick and it gives the FCC an indication of what the pilot wants to achieve; turn, climb, descend and so on. The FCC works out the fine details of how to do it because it requires a complex and coordinated movement of more than one control surface. The pilot cannot fly the aircraft without the FCC.
But the FCC can fly the aircraft without the pilot. It just needs to get its objectives from somewhere else. For example, a GPS-enabled autonomous drone just needs a destination and maybe a set of way-points along a route and it can fly itself there – and dynamically adapt to the unpredictable and invisible winds along the way that would otherwise blow it off a rigidly predefined plan.
So, how does all this relate to health care?
Well, the key to the success of fly-by-wire is the design of the feedback loop. It has to use the correct sensory information; that information needs to be accurate and up-to-date; and it needs to be processed quickly enough to respond proactively. By that I mean the FCC needs to be able to predict what will happen in the near future and to plan accordingly to achieve the objectives and avoid the obstacles. The effect is smooth, stable, fast and efficient flight that looks and feels effortless. But that is an illusion. It is not easy and it is not effortless. If a pilot tries to do it, even a moment of hesitation or a minor gust of wind will cause the craft to become unstable, spin out of control and crash.
A human pilot cannot sense, process, plan and decide what to do accurately or quickly enough. Even if the pilot’s decisions and actions are correct, they will come too-late and have the unintended effect of actually destabilising the system.
This metaphor translates to health care. If we attempt to “fly” the health care system using a top-down-command-and-manual-control design that is akin to the 1903 Wright Flyer I, then we will experience frequent instability and occasional crashes – just as the early aircraft did. And if the “weather” gets blustery then we are even less likely to be able to control our health care system that way. We have learned the hard way that we are safer staying in our “hanger” and doing nothing. But, an aircraft parked in a hanger is ineffective as a vehicle and a hospital constrained by fear-fuelled-do-nothing-top-down-command-and-control policies is ineffective as a vehicle for care delivery. Especially when unpredictable challenges appear – such as a global pandemic of a novel infectious disease.
So, if we reflect on the fly-by-wire metaphor we could ponder on what we might need in health care: Embedded multi-sensors; automated real-time sensory data communication and transformation; and accurate, fast feedback loops that connect directly to where the micro-decisions are made and the micro-actions happen. The front line of health care delivery.
And we do not actually need centralised control hardware and software (i.e. flight control computers) because they are designed for the predictable and passive world of aerodynamics where the Non-Negotiable Laws of Physics decree what happens.
We need to be able to adapt to shifting preferences and policies. And something we already have in our health care system is “distributed chimpware” – trained and experienced health care staff. This resource, when used effectively, is much better suited to the shifting subjectivity of day-to-day health care delivery.
Humans have evolved with a highly developed visual sensory system – so the more effective and efficient way to feed back the real-time information is as a dynamic picture of what has happened, what is happening and what is about to happen. And so long as that picture is accurate and up-to-date enough; and we have a clear enough objective; and we have learned a validated method for transforming the information into decision and action – then the health care delivery system can be trusted to fly itself. And it would.
But we don’t have that in health care. We have a fragmented health care system that cannot work in a coordinated and collaborative way because it was never designed to.
So, we are forced to fall back on our out-of-date, ponderous and potentially destabilising and dangerous top-down-command-and-control approach.
Question: Why haven’t we designed the health care system to be as safe, stable, efficient and trusted as a modern passenger aircraft?
Could it be because we don’t have embedded health care systems engineers who can design, build, implement and maintain such things?
But there is some hope that this is possible and some evidence that it is useful.
There are a small number of trained and experienced systems engineers working in the NHS today. They have been working behind the scenes to mitigate some of the effects of the COVID pandemic; and they have demonstrated the art of the possible.
One innovative solution is a drive-thru urgent primary care service in Birmingham where patients with urgent problems (i.e. not emergency or routine) can be referred by their GP or book themselves – and are seen and assessed safely and quickly and without queuing. The prototype was created very quickly at the start of the pandemic and it has proved so effective that it has been developed and implemented as a more permanent solution.
Part of the control system design challenge was to ensure that the clinical resource capacity was well utilised (i.e. delivered value for money) but was not over-burdened. Even with the unpredictable nature of unscheduled urgent demand.
So, one component of the system design is a real-time visual feedback loop that the service provider uses to dynamically balance requests with resources. The screenshot below is real and recent.
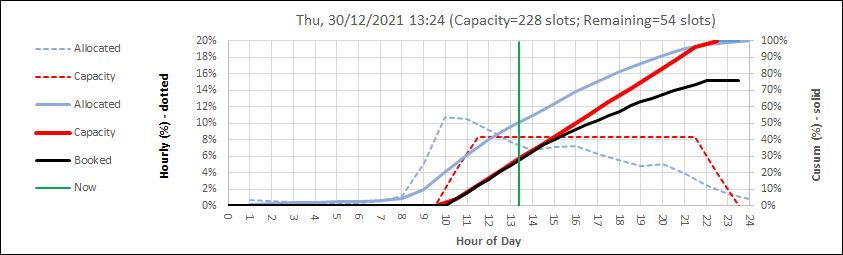
The dotted lines show the averaged historical pattern of hourly demand (blue) and flow-capacity (red) and these are used to create the solid lines which are cumulative sums. The green line shows ‘now’ so the past is to the left and the future is to the right. The black line is the current cumulative booked capacity and it cannot cross the red line (available slot-capacity) because the bookings are done on-line and a patient cannot attend without a ‘ticket’. Just as we do for trains, etc. The chart is updated automatically every 2 minutes so the service provider can see what is coming over the time horizon and use that information to dynamically tweak the process. This way, it is possible to achieve high utilisation (i.e. minimal waste of expensive and scarce clinical resources) while also avoiding chaotic queues and long, potentially unsafe, delays for patients.
So, maybe health care could use more of these aerospace engineering metaphors and grow some more health care systems engineers?
The growing body of evidence shows the art of the possible.
