If you put an ear to someones chest you can hear their heart “lub-dub lub-dub lub-dub”. The sound is caused by the valves in the heart closing, like softly slamming doors, as part of the wonderfully orchestrated process of pumping blood around the lungs and body. The heart is an impressive example of bioengineering but it was not designed – it evolved over time – its elegance and efficiency emerged over a long journey of emergent evolution. The lub-dub is a comforting sound – it signals regularity, predictability, and stabilty; and was probably the first and most familiar sound each of heard in the womb. Our hearts are sensitive to our emotional state – and it is no accident that the beat of music mirrors the beat of the heart: slow means relaxed and fast means aroused.
If you put an ear to someones chest you can hear their heart “lub-dub lub-dub lub-dub”. The sound is caused by the valves in the heart closing, like softly slamming doors, as part of the wonderfully orchestrated process of pumping blood around the lungs and body. The heart is an impressive example of bioengineering but it was not designed – it evolved over time – its elegance and efficiency emerged over a long journey of emergent evolution. The lub-dub is a comforting sound – it signals regularity, predictability, and stabilty; and was probably the first and most familiar sound each of heard in the womb. Our hearts are sensitive to our emotional state – and it is no accident that the beat of music mirrors the beat of the heart: slow means relaxed and fast means aroused.
Systems and processes have a heart beat too – but it is not usually audible. It can been seen though if the measures of a process are plotted as time series charts. Only artificial systems show constant and unwavering behaviour – rigidity – natural systems have cycles. The charts from natural systems show the “vital signs” of the system. One chart tells us something of value – several charts considered together tell us much more.
We can measure and display the electrical activity of the heart over time – it is called an electrocardiogram (ECG) -literally “electric-heart-picture”; we can measure and display the movement of muscles, valves and blood by beaming ultrasound at the heart – an echocardiogram; we can visualise the pressure of the blood over time – a plethysmocardiogram; and we can visualise the sound the heart makes – a phonocardiogram. When we display the various cardiograms on the same time scale one above the other we get a much better understanding of how the heart is behaving as a system. And if we have learned what to expect to see with in a normal heart we can look for deviations from healthy behaviour and use those to help us diagnose the cause. With experience the task of diagnosis becomes a simple, effective and efficient pattern matching exercise.
The same is true of systems and processes – plotting the system metrics as time-series charts and searching for the tell-tale patterns of process disease can be a simple, quick and accurate technique: when you have learned what a “healthy” process looks like and which patterns are caused by which process “diseases”. This skill is gained through Operations Management training and lots of practice with the guidance of an experienced practitioner. Without this investment in developing knowlewdge and understanding there is a high risk of making a wrong diagnosis and instituting an ineffective or even dangerous treatment. Confidence is good – competence is even better.
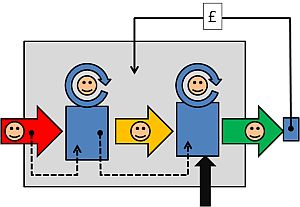
The objective of process diagnostics is to identify where and when the LUBs and HUBs appear are in the system: a LUB is a “low utilisation bottleneck” and a HUB is a “high utilisation bottleneck”. Both restrict flow but they do it in different ways and therefore require different management. If we confuse a LUB for a HUB and choose the wrong treatent we can unintentionally make the process sicker – or even kill the system completely. The intention is OK but if we are not competent the implementation will not be OK.
Improvement Science rests on two foundations stones – Operations Management and Human Factors – and managers of any process or system need an understanding of both and to be able to apply their knowledge in practice with competence and confidence. Just as a doctor needs to understand how the heart works and how to apply this knowledge in clinical practice. Both technical and emotional capability is needed – the Head and the Heart need each other.